The CMS Final Rule
“This Center of Medicare and Medicaid (CMS) Final Rule is intended to move the health care ecosystem in the direction of interoperability, and to signal our commitment to the vision set out in the 21st Century Cures Act and Executive Order 13813 to improve the quality and accessibility of information that Americans need to make informed health care decisions, including data about health care prices and outcomes, while minimizing reporting burdens on affected health care providers and payers” – CMS
As part of this new rule, CMS outlined specific changes to the Prior Authorization (PA) process to decrease the burden on providers and members, and improve coordination and quality of care (e.g., eliminating fax communications for authorizations). Because of the urgency and high visibility of this initiative, large to small size health plans nationwide are working diligently, performing operational assessments, and identifying gaps with resolutions to enrich their Utilization Management (UM) automation.
What is UM and how does automation fit into the equation?
Utilization Management (UM) is an objective process that involves providers requesting healthcare services prior to treatment known as Prior Authorization (PA) and payers using evidenced-based criteria to evaluate requested services to make fair and timely decisions resulting in an approval or denial. This process entails the collection of relevant clinical information submitted by providers and review by qualified health plan clinicians in alignment with regulatory mandates, policies, and procedures.
Automation is the ability for providers to electronically create and send authorization requests using a secured automated software system supporting the functions below:
- Creating authorization requests with unique member identifiers, diagnoses, and procedures needed
- Submitting supporting clinical documentation
- Decisioning based on evidenced based criteria with an immediate response
Current challenges influencing CMS ruling
The main challenges providers and payers face today involve delays in authorization decisions related to complicated phone/fax manual processes and overallocated clinical teams, placing members at risk for health complications due to delay of services. Although health plans have tried to implement high-quality interactive voice (IVR) phone systems, several issues exist with this solution including providers being routed at times to the wrong departments, extended hold times, and accidentally abandoned calls. Furthermore, reliance on inconsistent fax systems further impedes timely authorization of services. All of this leads to providers and payers unnecessarily expending resources, clinicians not working at the top of their license but rather bogged down in administrative tasks, and high volumes of pended authorizations.
Anoteros Automation Approach
Automating the Prior Authorization process requires payers and providers to work together to transform their business processes and implement robust technology. Here are some key steps and considerations for implementing an automated Prior Authorization process:
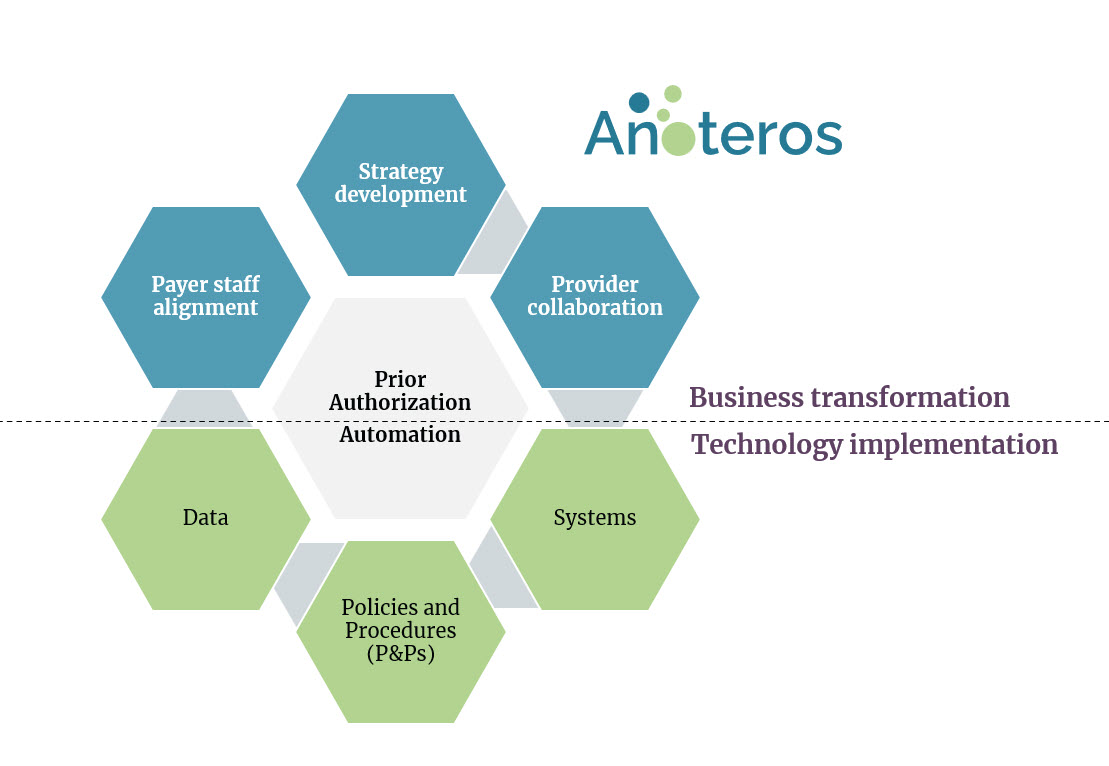
Strategy Development:
- Develop UM efficiency goals
- Set organizational mandates for automation
- Develop a roadmap for implementation
Provider Collaboration:
- Partner with the Provider community
- Understand Provider requirements
- Develop contractual obligations and incentives
- Educate Providers and manage change
Payer Staff Alignment:
- Work with staff on change mgmt. (Provider relations, UM, Claims, Appeals)
- Alleviate concerns about automation
- Review staffing model based on efficiency gains
Data:
- Use historical data to gain insights
- Categorize services (cost, volume, etc.)
- Make data-driven decisions for automation
Systems:
- Implement using industry standards and best practices
- Integrate Portal with Payer IT ecosystem (Provider Portal, UM, Clinical Guidelines, Claims)
Policies and Procedures:
- Research medical policies for automation
- Setup/revisit UM governance
- Review and update Policies and Procedures
- Develop Job-aides/ Desk Level Procedures
Anoteros has assisted several payers in implementing automation for prior authorizations in the past few years. These initiatives were complex business transformation efforts involving strategy, business process redesign, change management, and compliance.
Contact us to start a conversation.
